The most prevalent cystic tumours of the pancreas are intraductal papillary mucinous neoplasm (IPMN) and mucinous cystic neoplasm (MCN), which account for approximately 2% of pancreatic tumours. IPMNs are tumours of the pancreatic duct origin, characterized by the production of dense mucinous content and its secretion into the pancreatic ducts. IPMN is classified into three subtypes based on morphological characteristics: IPMN of the main pancreatic duct, IPMN of side branches, and mixed type of IPMN. MCN, on the other hand, typically occurs in middle-aged patients, and invasive cancer is present in less than 15% of patients. Distal pancreatectomy is the operative treatment of choice due to the age, general condition, and localization of these tumours in the body and tail of the pancreas. IPMN and MCN have malignant potential and may transform into invasive pancreatic cancer.
Risk factors for the development of cystic tumours of the pancreas include insulin-dependent diabetes, chronic pancreatitis, and a positive family history of pancreatic ductal adenocarcinoma.
Cystic tumours of the pancreas often present few symptoms. Obstruction of the pancreatic duct or the main bile duct may lead to abdominal pain, nausea, vomiting, jaundice, and greasy or light-coloured stools. The suspicion of a cystic tumour of the pancreas may arise from acute pancreatitis or newly diagnosed diabetes mellitus.
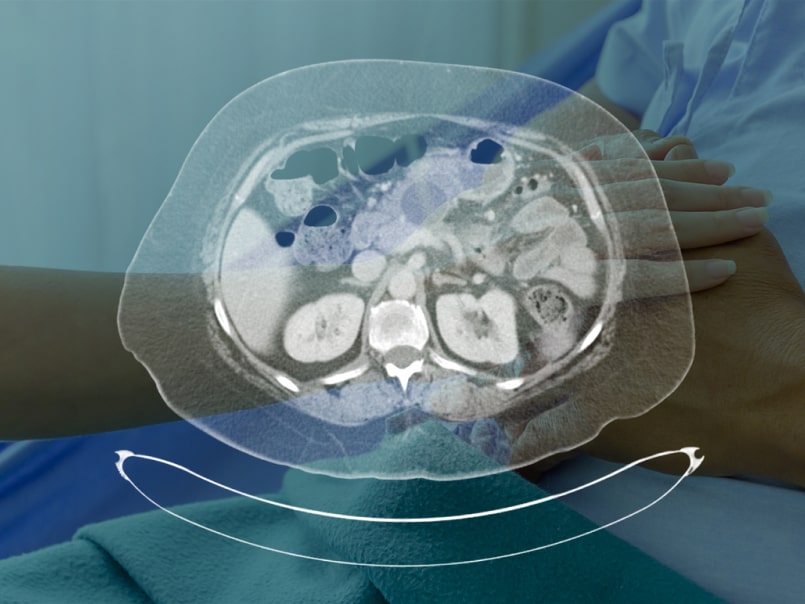
The diagnosis of pancreatic cystic tumours is typically made via radiological imaging, including magnetic resonance imaging of the abdomen, magnetic resonance cholangiopancreatography (MRCP), and computed tomography (CT) scanning. Endoscopic ultrasound is useful for obtaining samples of the cyst contents for cytological and genetic analysis.
High-grade dysplasia or invasive carcinoma is present in up to 60% of patients with IPMN of the main pancreatic duct, requiring operative treatment due to a five-year survival rate of 31-54%. Resection of the pancreas until a negative resection margin is achieved is the standard surgical treatment. Approximately 17% of patients with IPMN of the lateral pancreatic duct have invasive carcinoma, with an annual rate of confirmed malignancies around 20%. Regular follow-up is advised for these patients if the changes are less than 4 cm. Surgical treatment may be recommended for patients younger than 65 years with cysts larger than 4 cm. The choice of treatment is individualized, taking into account the general condition of the patient, the risk of malignancy, localization, and size of the tumour.
Genetic predisposition is a significant factor in the development of cystic tumours of the pancreas, which cannot be influenced. Smoking cessation and limited alcohol consumption may reduce the risk of developing these tumours. A healthy lifestyle, including a balanced diet, physical activity, and maintaining a healthy body weight, may reduce the risk of developing diabetes and subsequently lower the risk of cystic tumours of the pancreas.